
Click HERE to read the original article by Henry Abbott on the differences between how James and Wade run and the impact it may have on their performance and health.

Posted by Boston Sports Medicine and Performance Group on Mar 5, 2011 10:37:00 AM

Click HERE to read the original article by Henry Abbott on the differences between how James and Wade run and the impact it may have on their performance and health.

Topics: Guest Author, Health & Wellness
Posted by Boston Sports Medicine and Performance Group on Feb 27, 2011 2:53:00 PM
Recently I was asked about what to do during halftime to get the guys prepared for the 2nd half of play. Currently I don’t do anything (stretching/warmup) as a team or for an individual unless they ask or there is evidence that something isn’t right. We do some half-ass layup lines with 8 guys, while 4 players wait to be personally stretched by our AT for the 2nd or 3rd time....
Prior to the game we shoot from the 90-60 minute mark and stretch at the 30 minute mark for 5-6 minutes at a good pace. The rest of the time is to get shots up etc.
My initial thought is to continue with our layup lines and possibly a more structured shooting drill. I’ve thought about a team stretch but at this point, neurologically, they’re either turned on or not. This would be our 3rd or 4TH STRETCH OF THE DAY if you include shoot-around!!!!
This is a good question and I don’t think there is a right or wrong answer. It really depends on your situation and what the head coach will ALLOW you to do. One things for sure, the outcome and performance by your team in the 1st half will probably determine what you may be able to do with the team during half-time (unlike the pre-game movement prep which is typically a structured routine). If you are up by 10-20pts, you may be able to take the team through a “structured” movement/stretching routine (because the half-time talk may not be as long and psychologically, the head coach and players are feeling good). However, If you are losing by 10-20pts, you may only get 2 minutes and the coaches and players may want to do some quick “on-court” shooting because their focus is strictly on the game and executing their on-court strategy.
Personally, I would rather have my players especially the starters go through some “position specific” on-court movement/shooting drills (regardless of the available time). I want their focus to be strictly on the game and competing (personally, I don’t want to be a distraction). If players have individual needs then myself and the athletic trainer will address those issues.
Ray Eady
University of Wisconsin
Topics: Basketball Related, Art Horne
Posted by Boston Sports Medicine and Performance Group on Feb 20, 2011 6:36:00 PM

Recently I was asked about what to do during halftime to get the guys prepared for the 2nd half of play. Currently I don’t do anything (stretching/warmup) as a team or for an individual unless they ask or there is evidence that something isn’t right.
Prior to the game we shoot from the 90-60 minute mark and stretch at the 30 minute mark for 5-6 minutes at a good pace. The rest of the time is to get shots up etc.
My initial thought is to continue with our layup lines and possibly a more structured shooting drill. I’ve thought about a team stretch but at this point, neurologically, they’re either turned on or not. This would be our 3rd or 4TH STRETCH OF THE DAY if you include shoot-around.
What are your thoughts?
• Strength & Conditioning Coach
_______________________________________________________
I have thought about this before too – after 20 minutes of play, how much cool down is involved during halftime? How long has a guy been sitting prior to the half? In that case, is static stretching the warm tissue better post halftime better than another dynamic motion (perhaps for guys who didn’t play as much). How much work is necessary to re-raise the heart rate? Lots of questions hard to answer.
Another interesting concept that I had discussed with my former Ex. Phys. Instructor at Georgia was having guys who played major minutes ride a bike easy for 3 minutes or so (even if they get into foul trouble and will sit for 10 minutes in the first half). That way your body chews off the lactic acid it just produced as energy and it doesn’t get to settle in the muscle. A great idea but hard to convince coaches and players that it would work.
As with most of the other coaches, I have found that we don’t have enough time – guys want to get shots up. I may address a specific player off to the side but coaches and players want shots to get a feel for the second half.
• Michael Schweigert, Northwestern University
_______________________________________________________
At the high school level (I am at DeMatha) we have even less time… and usually return from the locker room with under two minutes on the clock… so I don’t do anything organized with the group. We rarely have time for lay-ups… our guys just head over the bench to get ready for the 2nd half. If a particular player has an issue – I address it.
I give our guys a handful of Gummi Bears at half-time – quick sugar to refuel their energy stores… no different than Gatorade or the orange slices we all ate as kids at the halftime of soccer games!
I let the team split two individual size bags… so each player gets about 6-8 Gummi’s.
• Alan Stein, DeMatha High School
_______________________________________________________
Great question! I have recently started a dynamic warm up right after our half time talk. Knee hugs, straight leg kicks, and anything else I could do in that amount of time. Since our rotation has been cut down I basically just have 7 to 8 guys going through this while everyone else is shooting. One major issue is your Head coach. Will they give you enough time? I would like if the guys did get up a couple of shots before the second half, because we are here for a basketball game. So if you do have enough time before the second half starts I think it’s a great idea. If your coach just tore the team a new one and gave you 2 minutes to return to the court then individual stretching may be the best bet.
• Ben Kenyon, George Washington University
_______________________________________________________
This is a good question and I don’t think there is a right or wrong answer. It really depends on your situation and what the head coach will ALLOW you to do. One thing is for sure, the outcome and performance by your team in the 1st half will probably determine what you may be able to do with the team during half-time (unlike the pre-game movement prep which is typically a structured routine). If you are up by 10-20pts, you may be able to take the team through a “structured” movement/stretching routine (because the half-time talk may not be as long and psychologically, the head coach and players are feeling good). However, if you are losing by 10-20pts, you may only get 2 minutes and the coaches and players may want to do some quick “on-court” shooting because their focus is strictly on the game and executing their on-court strategy.
Personally, I would rather have my players especially the starters go through some “position specific” on-court movement/shooting drills (regardless of the available time). I want their focus to be strictly on the game and competing (personally, I don’t want to be a distraction). If players have individual needs then I and the athletic trainer will address those issues.
• Ray Eady, University of Wisconsin
_______________________________________________________
I couldn't have said it better….they need to get shots up and if individuals need to be stretched then I can take care of them – but it depends on the game. Usually we'll head out with 2 or so minutes to go which isn't enough time to get loose again – they need more of a specific warmup….lay-ups, shots, etc.
• Brijesh Patel, Quinnipiac College
_______________________________________________________
Minutes 15-10:
focus on rehydrating with Water and Powerade, and replenishing blood sugar levels. We use Solobars cut in half so guys can either grab one or two pieces.
Minutes 10-5:
Coaches talk - address tactics and second half changes
Minutes 5-1:
Athletes return to court. With the four minutes remaining, our guys jump into some "trigger" shooting attempting to get as many "game" shots up as possible. I'll address any guys with personal stretching and some guys in the past have even jumped on a bike in order to re-break a sweat.
Minutes 1-0:
Coaches and Athletes huddle to address any last changes.
• Art Horne, Northeastern University
Topics: basketball conference, basketball training programs, athletic training conference
Posted by Boston Sports Medicine and Performance Group on Feb 13, 2011 3:04:00 PM

"When people say God blessed me with a beautiful jump shot, it really pisses me off. I tell those people, 'Don't undermine the work I've put in every day.' Not some days. Every day."
- Ray Allen
Topics: Basketball Related, basketball conference, athletic training conference, Ray Allen
Posted by Boston Sports Medicine and Performance Group on Feb 6, 2011 10:05:00 AM
Topics: Guest Author, Health & Wellness
Posted by Boston Sports Medicine and Performance Group on Feb 6, 2011 8:45:00 AM
A review of:
Using nitric oxide to treat tendinopathy. George A C Murrell. Br J Sports Med 2007 41: 227-231
By Art Horne

Below are a few points of emphasis worth noting when discussing this potentially helpful treatment option with your team physician and care group in regards to your basketball athlete and their patellar tendinopathy. Of course, treating the actual source of the patellar pain (hips, lack of ankle dorsiflexion, etc) is always preferred, many troublesome cases require some additional treatment approaches for athletes to get over the hump and back to high level jumping and basketball activities. Clinicians should read both this article in addition to other research articles related to the use of Nitric Oxide in the treatment of tendinopathy prior to considering this as part of your treatment protocol.
Let’s start at the end with the discussion:
DISCUSSION
“NO is important to tendon healing. All three isoforms of NOS, the enzyme that produces NO, are expressed by fibroblasts during tendon healing. Our data in animal studies, cell culture and clinical trails support the hypothesis that NO enhances extracellalar matrix synthesis and results in injured tendons having better material and mechanical properties – that is, the healing tendons are stronger on a per unit area basis than those not exposed to additional NO. The clinical trials show that delivering NO via a patch enhances the clinical recovery of tendinopathy, which is manifested by a reduction in pain, an increase in range of motion and an increase in strength.”
In the three trials outlined below, each used a commercially available NO delivery system (glyceryl trinitrate (GTN). “NO is important for the volume of tissue synthesized during tendon healing. NO is likely to be important in a number of processes, including local blood flow and host defense.”
TENNIS ELBOW
“The NO group had less tenderness and could perform more work and had greater power on the Orthopaedic Research Institute-Ankle Strength Testing System testing. The changes were most apparent at week 24. In all, 81% of patients receiving GTN patches were asymptomatic in activities of daily living at 6 months compared with 60% of patients with tendon rehabilitation alone”
ACHILLES TENDON
“The NO (GTN) group performed significantly better on hop testing and could generate more peak force at week 24. In all, 78% of patients receiving GTN patches were asymptomatic for activities of daily living at 6 months compared with 49% of patients with tendon rehabilitation alone.”
SUPRASPINATUS TENDINOPATHY
“This trial produced the most significant effects. The NO group had significantly reduced shoulder pain with activity and at night, improved range of motion in abduction, forward flexion and external rotation, and improved power in abduction, external rotation, subscapularis and supraspinatus. The changes in supraspinatus power were the most dramatic, and were significant at 6 weeks. In all, 46% of patients receiving GTN patches were asymptomatic for activities of daily living at 6 months compared to 24% of patients with tendon rehabilitation alone.
Points to consider and discuss with your care team:
• Although the treatment of knee pain and specifically patellar tendinopathy was not examined in this study, it may be a worthwhile treatment option in the future.
• It is important to note that in both the tennis elbow and Achilles tendinopathy that the most apparent results were noted at week 24.
• With that said, a treatment program involving Nitric Oxide would still require other treatment options in order to alleviate pain short-term.
• Patients should be advised that they may experience headaches while using the patches and blood pressure should be monitored for the first few days to ensure no adverse effects.
• For additional resources on Knee Pain and the Basketball athlete visit these links:
Treating Anterior Knee Pain by Professor Paul Canavan
Treating Anterior Knee Pain In The Basketball Athlete Part I by Art Horne
Treating Anterior Knee Pain In The Basketball Athlete Part II by Art Horne
Topics: Art Horne, Health & Wellness
Posted by Boston Sports Medicine and Performance Group on Jan 30, 2011 4:00:00 PM
Here is the situation:
You are in bright and early for an early morning practice. It about an hour and a half before the team’s 8:00am go time on the court. Normal practice prep is on your mind along with some rehabilitation notes you are documenting before the players arrive. One of the players happens to report a little early this morning with a distressed look on his face. You meet him at the treatment table and listen as the player describes an intense testicle pain. The pain is described as nothing he has ever felt before. He reports to your athletic training room with acute onset of unilateral scrotal pain, scrotal swelling, nausea, abdominal pain, fever, urinary frequency. He tells you he woke up with the pain and it has been getting worse over the course of the past 2 hours. Do you recognize the male medical emergency, if not this young man could potentially loose his testicle………
Given the population that Boston Sports Medicine and Performance Group reaches out to and focuses on it is important to examine male emergencies in men’s basketball. A male emergency all athletic trainers working with basketball should be aware of is testicular torsion.
Testicular torsion is a true urologic emergency and must be differentiated from other complaints of testicular pain because a delay in diagnosis and management can lead to loss of the testicle. Though testicular torsion can occur at any age, including the prenatal and perinatal periods, it most commonly occurs in adolescent males; it is the most frequent cause of testicle loss in that population.
Pathophysiology
The testicle is covered by the tunica vaginalis, a potential space that encompasses the anterior two thirds of the testicle and where fluid from a variety of sources may accumulate. The tunica vaginalis attaches to the posterolateral surface of the testicle and allows for little mobility of the testicle within the scrotum.
In patients who have an inappropriately high attachment of the tunica vaginalis, the testicle can rotate freely on the spermatic cord within the tunica vaginalis (intravaginal testicular torsion). This congenital anomaly, called the bell clapper deformity, can result in the long axis of the testicle being oriented transversely rather than cephalocaudal. This congenital abnormality is present in approximately 12% of males, 40% of whom have the abnormality in the contralateral testicle as well.1 The bell clapper deformity allows the testicle to twist spontaneously on the spermatic cord. Torsion occurs as the testicle rotates between 90° to 180°, causing compromised blood flow to the testicle.
Complete torsion usually occurs when the testicle twists 360° or more; incomplete or partial torsion occurs when the twisting is less than this. The twisting of the testicle causes venous occlusion and engorgement as well as arterial ischemia and infarction of the testicle. How tightly the testicle is twisted appears to correlate with how quickly the testicle becomes nonviable from ischemia.
Causes of testicular torsion may include the following:
• Congenital anomaly; bell clapper deformity
• Undescended testicle
• Sexual arousal and/or activity
• Trauma
• Testicular tumor
• Exercise
Emergency Department Care
• Early diagnosis and prompt urologic consultation is essential since time is critical in salvage of the testicle.
• Analgesic pain relief should be administered as testicular torsion is typically very painful.
• Attempt manual detorsion with pain relief as the guide for successful detorsion. The procedure is similar to the "opening of a book" when the physician is standing at the patient's feet.
• Most torsions twist inward and toward the midline; thus, manual detorsion of the testicle involves twisting outward and laterally.
• Consultation with urology is a must since most testicular torsion need surgical intervention.
The unique aspect of being an athletic trainer is that it involves being well educated on all aspects of medical emergencies in the population we provide care. Medical emergencies related to orthopedic and internal medicine. It is all about early recognition to provide efficient and appropriate care.
References
Dogra V, Bhatt S. Acute painful scrotum. Radiol Clin North Am. Mar 2004;42(2):349-63. [Medline].
Ringdahl E, Teague L. Testicular torsion. Am Fam Physician. Nov 15 2006;74(10):1739-43. [Medline].
Beni-Israel T, Goldman M, Bar Chaim S, Kozer E. Clinical predictors for testicular torsion as seen in the pediatric ED. Am J Emerg Med. Sep 2010;28(7):786-9. [Medline].
Cattolica EV, Karol JB, Rankin KN, Klein RS. High testicular salvage rate in torsion of the spermatic cord. J Urol. Jul 1982;128(1):66-8. [Medline].
Coley BD. The Acute Pediatric Scrotum. Ultrasound Clinics. 2006;1:485-96. [Full Text].
Hayn MH, Herz DB, Bellinger MF, Schneck FX. Intermittent torsion of the spermatic cord portends an increased risk of acute testicular infarction. J Urol. Oct 2008;180(4 Suppl):1729-32. [Medline].
Creagh TA, McDermott TE, McLean PA, Walsh A. Intermittent torsion of the testis. BMJ. Aug 20-27 1988;297(6647):525-6. [Medline].
Schmitz D, Safranek S. Clinical inquiries. How useful is a physical exam in diagnosing testicular torsion?. J Fam Pract. Aug 2009;58(8):433-4. [Medline].
Brenner JS, Ojo A. Evaluation of scrotal pain or swelling in children and adolescents. UpToDate [web site]. 2006.
Eyre RC. Evaluation of the acute scrotum in adults. UpToDate [web site].
Doehn C, Fornara P, Kausch I, et al. Value of acute-phase proteins in the differential diagnosis of acute scrotum. Eur Urol. Feb 2001;39(2):215-21. [Medline].
Prando D. Torsion of the spermatic cord: the main gray-scale and doppler sonographic signs. Abdom Imaging. Sep-Oct 2009;34(5):648-61. [Medline].
Dogra VS, Bhatt S, Rubens DJ. Sonographic Evaluation of Testicular Torsion. Ultrasound Clinics. 2006;1:55-66.
Yagil Y, Naroditsky I, Milhem J, Leiba R, Leiderman M, Badaan S, et al. Role of Doppler ultrasonography in the triage of acute scrotum in the emergency department. J Ultrasound Med. Jan 2010;29(1):11-21. [Medline].
Turgut AT, Bhatt S, Dogra VS. Acute Painful Scrotum. Ultrasound Clinics. 2008;3:93-107. [Full Text].
Cassar S, Bhatt S, Paltiel HJ, Dogra VS. Role of spectral Doppler sonography in the evaluation of partial testicular torsion. J Ultrasound Med. Nov 2008;27(11):1629-38. [Medline].
Blaivas M, Sierzenski P, Lambert M. Emergency evaluation of patients presenting with acute scrotum using bedside ultrasonography. Acad Emerg Med. Jan 2001;8(1):90-3. [Medline].
Bomann JS, Moore C. Bedside ultrasound of a painful testicle: before and after manual detorsion by an emergency physician. Acad Emerg Med. Apr 2009;16(4):366. [Medline].
Capraro GA, Mader TJ, Coughlin BF, et al. Feasibility of using near-infrared spectroscopy to diagnose testicular torsion: an experimental study in sheep. Ann Emerg Med. Apr 2007;49(4):520-5. [Medline].
Terai A, Yoshimura K, Ichioka K, et al. Dynamic contrast-enhanced subtraction magnetic resonance imaging in diagnostics of testicular torsion. Urology. Jun 2006;67(6):1278-82. [Medline].
Moschouris H, Stamatiou K, Lampropoulou E, Kalikis D, Matsaidonis D. Imaging of the acute scrotum: is there a place for contrast-enhanced ultrasonography?. Int Braz J Urol. Nov-Dec 2009;35(6):692-702; discussion 702-5. [Medline].
Baker LA, Sigman D, Mathews RI, et al. An analysis of clinical outcomes using color doppler testicular ultrasound for testicular torsion. Pediatrics. Mar 2000;105(3 Pt 1):604-7. [Medline].
Blank BH, Goldsmith G, Schneider RE. Recognizing a testicular emergency. Patient Care. 1997;31(13):117-35.
Brenner JS, Ojo A. Causes of scrotal pain in children and adolescents. UpToDate [web site]. 2006.
Caesar RE, Kaplan GW. Incidence of the bell-clapper deformity in an autopsy series. Urology. Jul 1994;44(1):114-6. [Medline].
Cattolica EV. Preoperative manual detorsion of the torsed spermatic cord. J Urol. May 1985;133(5):803-5. [Medline].
Flanigan RC, DeKernion JB, Persky L. Acute scrotal pain and swelling in children: a surgical emergency. Urology. Jan 1981;17(1):51-3. [Medline].
Kadish HA, Bolte RG. A retrospective review of pediatric patients with epididymitis, testicular torsion, and torsion of testicular appendages. Pediatrics. Jul 1998;102(1 Pt 1):73-6. [Medline].
McCollough M, Sharieff GQ. Abdominal surgical emergencies in infants and young children. Emerg Med Clin North Am. Nov 2003;21(4):909-35. [Medline].
Schwab R. Acute scrotal pain requires quick thinking and plan of action. Emerg Med Rep. 1992;13(2):11-7.
Wan J, Bloom DA. Genitourinary problems in adolescent males. Adolesc Med. Oct 2003;14(3):717-31, viii. [Medline].
Weber DM, Rosslein R, Fliegel C. Color Doppler sonography in the diagnosis of acute scrotum in boys. Eur J Pediatr Surg. Aug 2000;10(4):235-41. [Medline].
Topics: Health & Wellness, Eric Gahan
Posted by Boston Sports Medicine and Performance Group on Jan 30, 2011 8:57:00 AM
By Art Horne, MEd, ATC, CSCS
This past week Mike Reinhold posted some thoughts on Squat Technique and Back Extensor Muscle Activity . His article got me thinking about squatting and the basketball athlete. Coming from Boston University and being heavily influenced by Glenn Harris, who does an excellent job with his guys there along with Mike Boyle who continues to train the ice hockey team, I preached the importance of the front squat to the basketball community and anyone that would listen at Northeastern for probably my first six years. Although Reinhold’s article focuses on erector spinae muscle activation primarily, I think it’s also worth noting the positives and negatives of each squat variation as it relates to the tall guys, especially incoming freshmen.
Like I said, for almost my first six years working with basketball we worked on front squatting, and front squatting only – the following was my defense:
• It’s the finish position for the clean (even though I never taught or trained this movement) and therefore teaches the athlete this position prior to actually encountering it under a moving load.
• Once technique failed either at the end of a set or during testing the athlete could simply dump the weight and avoid the dreadful “good morning” posture commonly seen with the back squat under heavy loads, thereby saving their back (whether this was the case or not, back pain cases within our team steadily declined to almost zero as each year passed).
• Guys with long tibias and femurs just seemed to be able to sit deep and with great form and little coaching. It was simply an easier movement to teach, coach and succeed with. Maybe because the front squat is a little bit more quad dominant and therefore the basketball athlete seems to be more at home and comfortable while performing this movement.
• Nothing looks more like a baby squat than a front squat – no, back squats don’t look quite the same – close – but not quite

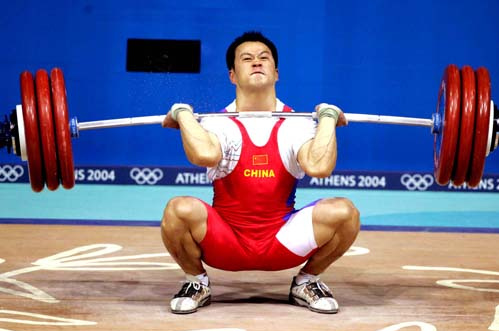
Front Squats sound good right?
Some points you may want to consider in favor of the back squat over the front squat for the basketball athlete:
• As Mike Reinhold mentioned, erector spinae is increased in with the front squat - this might be ok if you're look to develop overall erector spinae strength, but not ok in novice lifters or athletes with previous low back pain.
• As I mentioned earlier, most basketball athletes, ok, all basketball athletes are quad dominant and with this usually comes some sort of anterior knee pain, most notably patellar tendinopathy, or good ol’ fashion “jumpers knee”. As Charlie Weingroff mentioned at the Basketball Symposium last year, maintaining a vertical tibia helps put the stress on the glutes and takes it off the knees – which for the basketball athlete and all knee pain victims across the country is a good thing. Although a true vertical tibia is almost impossible during squatting, and rarely the position during any incredible athletic event, getting closer to vertical than not certainly reduces the reports of knee pain during squatting activity and I consider that a good thing – this of course is more easily achieved through the back squat or box squat than the front squat.
• As loads progressed with the front squat, and specifically with incoming athletes, the load was limited by the amount of strength their upper body could hold, and not their lower extremity. Imagine doing chin-ups and your grip failing before your back was able to benefit from the exercise. This is exactly what ended up happening with some of our athletes. Their erector strength and overall upper body simply couldn’t handle the loads and thus missed out on the intended training effect for the lower extremity.
• As each year passed, and a new version of the Iphone and Madden NFL football was released, our basketball athlete's posture declined at a most painful rate and putting someone under the bar in a bad loaded posture started to look worse and worse with the front squat. At least with the back squat, so long as they had normal shoulder mobility, athletes were automatically placed in what I would consider a much more favorable posture (and thoracic position) under load.
• Lastly, and probably most importantly, guys rarely experienced glute soreness with the front squat. We all know glutes are King and if I wanted to really and truly establish a great training base while also avoiding the potential of exacerbating existing knee pain – back squatting was going to have to be introduced.
Ultimately, this debate lead me to following Dr. Stu McGill around one conference until he was kind enough to answer the following question, “Which is better for BASKETBALL ATHLETES, front or back squat.”
“In terms of back health, it has to be the back squat,” Stu responded.
He didn’t really answer my question and I didn’t get around to pestering him as to why that day, but since then and through corresponding with him, I would imagine one of his main points is the opportunity to “bend the bar” over your back and engage and utilize the large lats as a lumbar stabilizer under heavy loads. Something you simply can’t do with the front squat.
I still don’t have an answer as to what squat technique is better for the BASKETBALL ATHLETE. Some tall guys absolutely crush the front and the back squat, while others can barely stand up against a stiff breeze. Whichever one you decide to go with keep in mind some general guidelines that I go by:
1. Don’t start kids off wearing belts to squat. If they can’t handle loads without the belt that means they can’t handle the load. Max testing – maybe. All other times leave the belts hanging up in the corner.
2. Previous back injury : back squat only, and probably with a belt if you squat at all – the risk-reward might just not be there. Talk to all parties involved in the care of the athlete when making this decision.
3. Ongoing knee pain: back squat and probably squat to a box and hammer vertical tibia position.
4. Super tall femurs – might just be better at the front squat. It doesn't mean they shouldn't back squat, but they may have to squat to a box.
5. Freshmen – great opportunity to teach both. Chances are they’ve never been taught, and if they were it was bad. Take the time and groove the crap out of each pattern and set them up to be successful studs come their junior and senior years. Everyone wants success right away, but squatting over the course of a college career works much better if you boil the frog.

Topics: Art Horne, Strength Training
Posted by Boston Sports Medicine and Performance Group on Jan 23, 2011 11:01:00 AM
Topics: Health & Wellness, Craig Liebenson
Posted by Boston Sports Medicine and Performance Group on Jan 23, 2011 10:50:00 AM

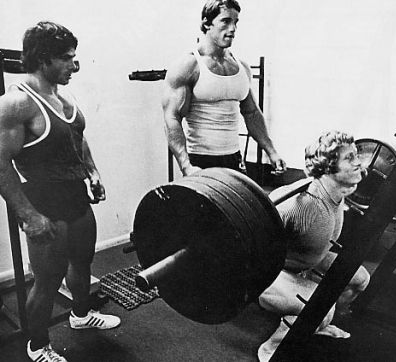
For the past three months I have been dedicating my Saturdays to an incredible program called Inner City Weightlifting. The program takes young people who are on a direct path to gang involvement and provides them with opportunities to participate in the sport of Olympic Lifting. Inner City Weightlifting provides students with career opportunities working for the nonprofit itself and in the field of personal training. The sport, coaches, and atmosphere facilitate a positive change for these students. As a student attempts to set a new personal record (PR) for weight lifted, everyone stops and watches. The lifters help ‘pump up’ the student’s morale and something unexpected happens: children who have been given limited support outside of a gang, are now encouraging each other, and a bond and team is formed. Every Saturday I look forward to spending time with this group of amazing young people and am reminded of the power of believing in the potentiality of others.
Stories demonstrating the success of the program
One student came to us 2 months ago. He was a member of one of the most high-profile gangs in Boston, and had been in and out of jail since his early teens. In January, 2010 he was shot 5 times in the torso. He was left paralyzed from the waste down, and homeless.
When we first started working with him, his future was dim. Over the last two months, however, his attitude has changed. We found him a job opportunity working with us, he is considering furthering his education, and he has made incredible progress in the strength and motion of his legs.
A few weeks ago, we got a call from his caseworker at Boston Medical Center. In the background we heard his voice shouting "ask them how many pull ups I do now!"
At the next practice he approached the coaches. He was getting papers signed, so we can work closely with his psychiatrist as well. Our coaches said, "Of course. Always let us know if there is anything we can do to help."
His response, "You already are."
Another story about one of our students….
“Eduardo” grew up on streets claimed by MS-13. He joined the gang at age 13. By 14, he was locked up for a year. Upon release he was stabbed and jumped several times. He faces an almost overwhelming pull to return to a life of violence.
Eduardo was under house arrest when we met. We set up equipment in his basement. At this time he was considering dropping out of school. During our sessions he spoke about what he had been through. We listened. At his next court appearance we lobbied his probation officer to let us work with him in a proper training facility.
Eduardo has been training at our gym for four months now. In truth, he has a chance. He’s set a goal of lifting more weight than anyone else in his weight class. He’s begun to speak about turning his grades around and attending Michigan State. Lifting, he’s told us, is his way to stay out of trouble. It is something he cannot do drunk or stoned. He cannot be at the gym and wandering the streets simultaneously. Eduardo now wants to come to practice every day.
Program Update
The biggest obstacle which we are facing at Inner City Weightlifting is finding facilities where we can bring our students to train. Many facilities have closed their doors after learning more about the students we work with and what backgrounds they have. Less than 1% of the population in Boston is responsible for more than 50% of the youth violence. Inner City Weightlifting is providing these youth with the confidence to say no to violence and yes to opportunity. It’s amazing what can happen if we open the doors for opportunity.
Links and Videos
Here is a news clip which aired on Channel 5
http://www.thebostonchannel.com/news/26134469/detail.html
Here is a link to the Inner City Weightlifting website
http://www.innercityweightlifting.org/
-Sarah Cahill
Topics: Basketball Related, Guest Author
© 2020 Boston Sports Medicine and Performance Group, LLC