
Symmetry and asymmetry are natural occurrences in sport, but the real insight to what is acceptable and what is an injury risk is unknown in the research on clinical ranges of motion, Electromyography, strength and power evaluation, and video analysis. One of the primary reasons Electromyography (EMG) is revealing is the specific details of why asymmetry may be present when visually the athlete appears to be symmetrical. What we do know is that asymmetry with injury is a valid etiology to muscle groups and joints of the lower extremity. Electromyography can easily add value to any existent movement screen or evaluation method or assist in designing new assessments if needed.
Etiology of Injury and Return to Play Strategies
Athletes may not be prone to injury just because of one imbalance or asymmetry, but as more factors elicit an symmetry, the probability increases. It is widely accepted that when an athlete is injured he or she will need the injured limb to exhibit less than a 10% deficit (1,2) between the uninjured limb, especially on strength. Maintaining symmetry is not just ensuring the strength is equal between limbs or sides, it's also important that range of motion and coordination is following the same guidelines. Removing symmetries is about reduction versus prevention, since most athletes will have anatomical and other technique styles that may encourage internal asymmetry. Performance and and medical specialists are to manage areas that may not be high risk and find areas that are likely culprits to the problems of non-contact injury, such as joint overuse syndromes and muscle strains. Following the 10% rule is a bit arbitrary as athletes in movement are not relying on just one muscle or system to create motion, but creating symmetry by revealing incomplete rehabilitation or unwanted training responses is necessary. While 10% may not be a true threshold, the act of measurement may reveal even higher deficits in functional movement such as jump tests, screening activities, and full sport movements. The goal of comparing limbs, especially the lower extremities, is to decrease the rate of injury by finding clear flags for further investigation. Injuries are common, but the they are often avoidable, especially in non-contact form.
Adding Surface Electromyography to Screening and Sport Movement
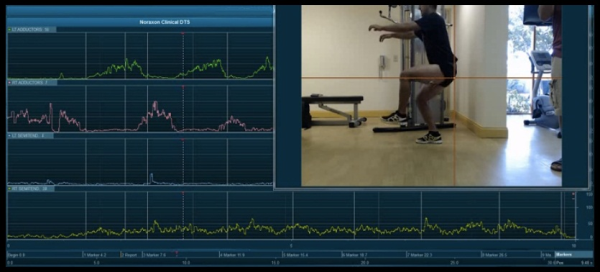
Visual compensations may not be present when significant neuromuscular dysfunction is present, due to the fact that most movements are a composite of multiple muscles systems. Flexibility, isolated strength, jump or movement tests, are all highly visible and most qualitative and quantitative information is limited by what the clinicians see. Other important insight is not visible, and kinetic data or EMG is a way to see what is below that surface. Coordination is hard to see, just the end result of motion, not the individual messages from the brain. Information from EMG shows activity of muscle groups or the lack of recruitment in joint activities, even when the resultant movements look normal. By looking below the surface a practitioner can see the root issues as symmetry visibly may be misleading when a specific firing pattern could be causing pain or malperformance. Noraxon <insert product> provides support to the the following options.
(1) Movement Screening- Any screen can be enhanced with EMG when used in combination, since movements are the result of the functional state of the neuromuscular system. Symmetry visually can be audited by the added data of EMG and determine if the movement screen is providing false negatives, common with athletes that are doing low force mobility screens. Movement screens can enhanced with incrementally higher speeds and forces to find what specific thresholds that can be problematic for that specific athlete, and improvements in training and therapy will raise the scorers over time if done properly.
(2) Power Tests- Simple lower, upper, or total body power tests are excellent ways to see if a functional imbalance is present with athletes. Power tests are normal part of training and athletes are comfortable doing them without any specific preparation or instruction. With absolute power tests coaches can combine risk factors with performance measures to get more information with the same tests, something especially necessary with limited time.
(3) Rehabilitation Exercises- Exercises in sports medicine studies are frequently validated with the use of EMG. Unfortunately many of the studies use exercises or movements that are not the options medical and performance staff need, and a gap exists to what is happening precisely besides estimated visuals. Sports therapists can create their own libraries of exercises and their variances internally when EMG is added to the movements.
(4) Sporting Actions- The most straightforward approach to evaluating possible dysfunctional movement or injury risk to look at the sporting movements the athlete is doing in practice or game simulation to see if something is compromised. Sporting actions are familiar with nearly everyone, so glaring problems can be clearly identified and knowledgable sport coaches can be part of the collaborative process.
In conclusion, the use of surface EMG is a gold standard in both performance and in modern rehabilitation. EMG explores and reveals what is beneath the surface visually and presents meaningful data when making comparisons in symmetry that could be troublesome if beyond the ability of the athlete.

References
- 1. Augustsson J, Thomee R, Karlsson S. Ability of a new hop test to determine functional deficits after anterior cruciate ligament recon- struction. Knee Surg Sports Traumatol Arthrosc. 2004;12:350-356.
Orchard J, Best TM, Verrall GM. Return to play following muscle strains. Clin J Sport Med. 2005;15:436-441.


