by Art Horne

Just recently Dr. Stuart McGill, Jordan Andersen and myself published an article in the Journal of Strength and Conditioning Research examining the link between traditional pre-season strength, fitness, and sports medicine testing to overall on-court basketball performance and injury resilience throughout the course of two collegiate basketball seasons. Although I would be the first to admit that there are some clear limitations to this study (number of participants for example), key performance predictors (points scored, ability to rebound, block shots, etc) were NOT associated with traditional strength or performance measures so often pursued in collegiate basketball strength programs.
Over the course of the next few weeks I will review this article in detail and provide insight into how actual on-court basketball performance may be improved upon beyond simply finding better parents or recruiting.
Predicting Performance and Injury Resilience From Movement Quality and Fitness Scores in a Basketball Team Over 2 Years
McGill, Stuart M.1; Andersen, Jordan T.1; Horne, Arthur D.2
Journal of Strength and Conditioning Research
July 2012
Introduction
The ability to successfully predict injury resilience and competition performance from preseason testing is a very wishful goal; however, questions remain regarding this objective: Do tests of fitness have a predictive ability for injury and are there other factors that can be assessed that may predict injury? Are there specific indicators that predict performance? This study was motivated by these questions.
Attempts to understand injury mechanisms and performance sometimes consider links to fitness. Traditionally, fitness testing, at least in occupational settings, has included the assessment of strength (13), joint range of motion (ROM) (23), and physiological variables such as heart rate, blood pressure, and oxygen uptake (2), but the performance scores in the occupational context are difficult to quantify. In contrast, there have been some studies relating fitness to sporting performance that are more tangible. In studies of ice hockey players (6,24), success could be more tangibly quantified from on-ice measures such as total minutes played and scoring chances. Green at al. stated that “goals scored” was not the best measure of hockey skill. Studies of football players suggest that those who score higher on movement quality tests have few injuries (11,12); however, preseason football combine testing is dominated by tests of strength and running speed. Recognizing that movement asymmetry and compromises to neuromuscular control have been linked to both future injury (11,12) and with having a history of back injury (17), movement assessments have been developed (3,4) and have been suggested to predict injury rates. Further, several fitness and movement tests have been implicitly assumed to predict “playing” performance by their inclusion into standard preseason tests. These include tests of endurance, strength, joint ROM, agility, and speed. The question remains as to the validity of these factors when attempting to predict injury resilience and performance.
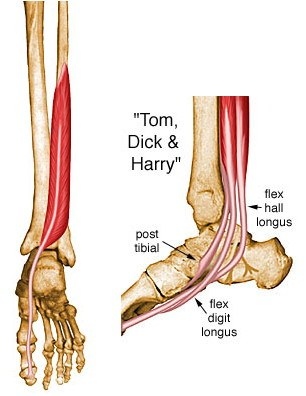
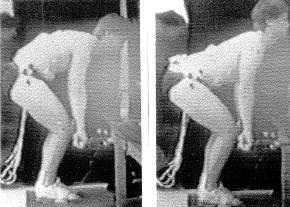
Although links between moving well and injury resilience and performance seem intuitive, this notion remains controversial. Interestingly, some evidence suggests that fitness training alone may not ensure peak performance or injury resilience (8,20). In addition, movement quality has been suggested to predict future injury (12). A possible mechanism may be that injury changes the way a person moves as an accommodation to pain (consider, e.g., the changes in mechanics throughout the anatomical linkage when limping from foot pain). Having a history of injury, in particular back injury, appears to change movement patterns (17). Movement patterns determine important injury criteria, such as joint and tissue load, together with influencing the length of time and repetitions an individual is able to perform a task with uncompromised form. Compromised form exposes the tissues to inordinate load elevating the risk of injury. Several examples of this link are available, for example, not maintaining a neutral curve in the lumbar spine while bending and lifting decreases the tolerable load at injury (in this case tissue failure [18]); having restricted hip motion is linked to having more spine motion when bending (17). Movement competency has also been linked with anterior cruciate ligament (ACL) injury rates, for example, having larger knee abduction moments and angles when landing from a jump predicted higher ACL injury rates (9). Given the variety of considerations for interpreting the links between movement, fitness, performance, and potential injury, the goal of this study was to first evaluate some traditional fitness test scores in a controlled athletic group that has a variety of challenging movement demands and also perform an assessment of the quality of movement. It was hoped that following a test group for a period of time would reveal links between specific fitness scores and movement quality with variables to predict injury resilience and performance. If such links exist, they could form a rationale for specific tests to be included in preseason testing.
The purpose of this study was to see if specific tests of fitness, and movement quality, could predict injury resilience and performance in a team of basketball players over 2 years (playing seasons).
It was hypothesized that in a university basketball population, (a) Preseason movement quality and fitness scores would predict in-season performance scores. (b). Preseason movement quality and fitness scores would predict in-season injury resilience.