Watch highlights from Cal Dietz's 2011 BSMPG summer seminar presentation.
Cal's entire presentation will be available for purchase shortly on BSMPG. Stay tuned for details.
Posted by Boston Sports Medicine and Performance Group on Fri, Oct 21, 2011 @ 09:10 AM
Topics: BSMPG, athletic training conference, boston hockey summit, athletic training, athletic training books, Cal Dietz
Posted by Boston Sports Medicine and Performance Group on Wed, Oct 19, 2011 @ 07:10 AM


Clare C. Frank DPT, MS, OCS, FAAOMPT
Dr. Frank received her physical therapy degree from Northern Illinois University. She completed the Kaiser Permanente Orthopedic Residency program in 1993 while working on her Master of Science degree in Physical Therapy at University of Southern California. She received her post-professional doctorate degree from Western University of Health Sciences, Pomona, California 2004. She is a board certified specialist in Orthopedic Physical Therapy and a fellow in the American Academy of Orthopedic Manual Physical Therapy. Her clinical career has been greatly influenced by Shirley Sahrmann PT, PhD, and the Prague School of Manual Medicine faculty, namely, the late Vladimir Janda MD, Karel Lewit MD, and Pavel Kolar PT, PhD.
Dr. Frank practices at a private clinic in Los Angeles, California. She has been instrumental in setting up the Movement Science Fellowship at Kaiser Permanente, Los Angeles. She has served on the medical team for the 2009 World Figure Skating Championships in Los Angeles, as well as the injury prevention team for the Chinese Olympic Teams 2010/11. She currently teaches in the U.S. and internationally and has co-authored “Assessment and Treatment of Muscle Imbalances: The Janda Approach”

Marcela Safarova PT, PhD
Dr. Safarova received her physical therapy training and completed her doctoral studies from Charles University. She is the head physiotherapist at Motol Hospital, a large teaching hospital associated with Charles University in Prague, Czech Republic. Dr. Safarova specializes in the rehabilitation of the locomotor system. She is also a certified Vojta therapist and has trained and works with both Professors Pavel Kolar and Karel Lewit. She also serves as an adjunct lecturer for both medical physiotherapy students at the university. She currently serves as an instructor for Professor Kolar’s courses both in Prague and internationally
ATTENTION: This course is limited to 30 seats only! Once seats are filled registration will close. Sign up before you miss this once in a lifetime learning opportunity.
Topics: basketball conference, basketball training programs, BSMPG, athletic training conference, Craig Liebenson, Charlie Weingroff, Barefoot in Boston, Clare Frank, DNS
Posted by Boston Sports Medicine and Performance Group on Mon, Oct 17, 2011 @ 07:10 AM
"Heads Up to Clinicians: Addressing Concussion in Sports among Kids and Teens" is a free, online course, developed by CDC through support from the CDC Foundation and the National Football League, available to health care professionals. It features interviews with leading experts, dynamic graphics, and case studies and provides an overview of what you, as a health care professional, need to know about concussion among young athletes.
Topics: Basketball Related, BSMPG, athletic training conference, athletic training, athletic trainer
Posted by Boston Sports Medicine and Performance Group on Thu, Oct 13, 2011 @ 09:10 AM
BSMPG is proud to annouce the first Dynamic Neuromuscular Stabilization course on the east coast this coming March 30th through April 1st, 2012.

The “Prague School of Rehabilitation and Manual Medicine” was established by key neurologists/physiatrists, all of whom were giants in the 20th century rehabilitation era i.e. Karel Lewit and the late Professors Vaclav Vojta, Vladimir Janda & Frantisek Vele. Based on groundbreaking neurodevelopmental and rehabilitation principles by these men, Professor Pavel Kolar has successfully integrated the work of his predecessors in proposing the underlying neurodevelopmental mechanism for how the movement system develops hand-in-hand with CNS maturation. This complex approach is “cutting-edge” in that it provides a window into provides a window into the complexity and plasticity of the CNS and its effect on the movement system. The DNS approach can be used in the rehabilitation of a myriad of neurologic, musculoskeletal pain syndromes as well as performance athletic training.
ATTENTION: This course is limited to 30 seats only! Once seats are filled registration will close. Sign up before you miss this once in a lifetime learning opportunity.
Topics: athletic training conference, athletic training books, Clare Frank, DNS course, DNS, dynamic neuromuscular stabilization
Posted by Boston Sports Medicine and Performance Group on Wed, Oct 12, 2011 @ 06:10 AM
I have to admit I missed the boat on the importance of manual medicine for a long time. After speaking to the best clinicians and therapists in the area there was one book that each and everyone of them, regardless of their current treatment approach, recommended I read - Greenman's Principles of Manual Medicine (Point (Lippincott Williams & Wilkins))
After recently completing this book I now know why. This book is a must for anyone treating musculoskeletal dysfunction on a daily basis. Below is a short excerpt from this book.
The Manipulable Lesion
"The acceptable term for this entity is somatic dysfunction. It is defined as impaired or altered function or related components of the somatic (body framework) system; skeletal, arthrodial, and myofascial structures; and related vascular, lymphatic, and neutral elements. Notice that the emphasis is on altered function of the musculoskeletal system and not on a disease state or pain syndrome." pg 11
DIAGNOSTIC TRIAD FOR SOMATIC DYSFUNCTION
"The mnemonic ART can express the diagnostic criteria for identification for somatic dysfunction.
“A” stands for asymmetry of related of the musculoskeletal system, either structural or functional.
“R” stands for range of motion of a joint, several joints, or region of the musculoskeletal system. The range of motion could be abnormal by being either increased (hypermobility) or restricted (hypomobility). The usual finding in somatic dysfunction is restricted mobility, identified by observation and palpation using both active and passive patient cooperation.
“T” stands for tissue texture abnormality of the soft tissues of the musculoskeletal system (skin, fascia, muscle, ligament, etc.). Tissue texture abnormalities are identified by observation and a number of different palpatory tests.
Some authors add one of two other letters to this mnemonic. “P” or a second “T”. “P” stands for pain associated with other findings, and “T” stands for tenderness on palpation of the area. Tenderness is particularly diagnostic if localized to a ligament. A normal ligament is not tender. A tender ligament is always abnormal. However, both pain and tenderness are subjective findings instead of the objective findings of symmetry, altered range of motion, and tissue texture abnormality. By the use of these criteria, one attempts to identify the presence of somatic dysfunctions, their location, whether they are acute or chronic, and particularly whether they are significant for the state of the patients wellness of illness at that moment in time. In addition to the diagnostic value, changes in these criteria can be of prognostic value in monitoring the response of the patient, not only to manipulative treatment directed toward the somatic dysfunction, but also to other therapeutic interventions." Pg 11-12
Topics: Art Horne, basketball performance, basketball resources, BSMPG, athletic training conference, boston hockey summit, boston hockey conference, barefoot strength training, barefoot training
Posted by Boston Sports Medicine and Performance Group on Mon, Oct 10, 2011 @ 06:10 AM

This past June Mark Toomey and Dr. John DiMuro presented at the BSMPG summer seminar, "Standing On The Shoulders Of Giants." Below is a small portion of Mark's most recent interview.
"We presented a paper together at Boston University and Northeastern University in June on fostering collaborative efforts between medical and exercise professionals. We "knuckle draggers" and I'm proud to call myself that, don’t have to play doctor. There are medical professionals who desire a relationship with us as long as we let them know what we're good at. My swim lane is only this wide but it’s this deep. I don’t want to be a doctor, I don’t want to be a healer - that’s a physician's job. But there is a legitimacy that creating a relationship with the medical community can give us."
Continue to read this interview on Dragondoor.com by clicking HERE
Topics: Art Horne, athletic training conference, athletic training, athletic training books, Mark Toomey, Barefoot in Boston, Dr. DiMuro
Posted by Boston Sports Medicine and Performance Group on Sat, Oct 8, 2011 @ 07:10 AM
By Art Horne

We’ve all done it from time to time – missed lunch to work with an athlete, stayed up late to write notes on the previous day’s work or ignored a pending physician or dentist appointment because we just didn’t have time.
And although it’s usually celebrated by those you care for and rewarded by the boss everyone knows this downward cycle of ignoring one’s own health in favoring of attending to the health of others can only be headed in one direction.
So the next time you board a plane when traveling remember to listen to your flight attendant’s very important message,
“During a change in altitude, oxygen masks will drop down from the ceiling. For patients travelling with young children, be sure to put your mask on first before helping your child.”
As busy as we all are it’s important to remember that the health of those we provide services for is inherently tied to our very own. It’s tough to continue to help others if you haven’t first helped yourself.
Topics: Art Horne, basketball conference, BSMPG, athletic training conference, athletic training books, barefoot strength training
Posted by Boston Sports Medicine and Performance Group on Fri, Oct 7, 2011 @ 07:10 AM
This past summer I was honored to be asked to team up with Brijesh Patel and contribute to Craig Liebenson’s upcoming function training text book. Craig is a health care provider that understands the need for both rehabilitation and serious strength training in order to perform at the highest level while reducing the chance of injury.
In short, Craig “gets it”.
Recently I was able to watch Craig’s most recent contribution to the health and performance field, his 3-disk DVD set.
Functional Performance Training
Flexibility, Yoga Training & Postural Advice DVD
This 3-DVD set is a great addition to all sports medicine libraries as Craig is able to bridge the gap between basic sports medicine rehabilitation exercises all the way to high level training with clear examples and coaching details. It has been my experience that it is this very gap that so many athletes either reinjure themselves or simply never get out of and thus fail to transition to elite sports performance altogether. The exercises that Craig outlines can be used in both rehabilitation settings or any high performance training center.
I was particularly impressed with both Craig’s respiration assessment and lower belly breathing exercises, which so many clinicians fail to evaluate and implement during their primary physical exam, along with Craig’s exercise selections and progressions within the Core Stability Training DVD. Because low back pain is nearly inevitable for all of us, and a certainty among college basketball athletes at some time during their college career, a working knowledge and a mastery of appropriate exercise selection is a paramount. The exercises outlined in this DVD are a must for all athletes as part of their general physical conditioning prior to low back pain or as part of their comprehensive core strengthening program after an episode of low back pain.
Topics: athletic training conference, Craig Liebenson, Barefoot in Boston, DNS course, Announcements, Core Stability Training, Functional Performance Training, Flexibility, Yoga, Postural Advice
Posted by Boston Sports Medicine and Performance Group on Thu, Oct 6, 2011 @ 07:10 AM
By Art Horne

So often ankle dorsiflexion or should I say a lack thereof, is pointed at as the underlying culprit for a variety of movement impairments … and rightfully so. A lack of true talocrural motion can cause havoc up the chain involving itself in a variety of impairments including anterior tibial pain, patellofemoral pain and general low back pain to only name a few.
However, the actual limiting factor causing this lack of osteokinematic motion may be multi-factorial and if clinicians are hoping to address this limitation over the long haul with permanent change the exact location and tissue responsible for this restriction must be clearly identified and addressed with a specific intervention to match the specific tissue.
With regards to soft tissue restrictions there are only 6 possible structures that can limit this motion, and these are:
1. Soleus
2. Posterior Tibialis
3. Flexor Hallucis Longus
4. Flexor Digitorum Longus
5. Posterior Talofibular ligament
6. Posterior Tibiotalar Ligament
The gastrocnemieus, although probably the very first structure that comes to mind, does not limit true dorsiflexion in function (that is unless you participate in ski jumping or speed walking, and then you need to include this in your assessment), since the knee is almost always flexed when the ankle is asked to express dorsiflexion in function, such as walking, running, squatting, lunging, stepping, jumping and landing.


Now that’s some dorsiflexion!
Remember, in order for your tibia to pass over your talus, and your talus to move between the tibia and the calcaneus we need to think of what pathology or dysfunction is not allowing the above mentioned tissues to lengthen. More often than not, fibrotic adhesions within the muscles or fascial restrictions are to blame, with the filet mignon of tissue treatment choice being an Active Release Technique. Although lesser cuts of treatment choices allow tissues to mobilize at times, rarely can a foam roller or tennis ball address a specific adhesion like a skilled clinician and the appropriate manual release technique. That’s not to say one is wasting their time or shouldn’t employ the soft tissue mobilization techniques that they are allowed to use given their credentialing or state laws, but understanding when to refer to a specialist with a very specific skill set is the difference between a butter knife a ninja – both may get the job done but we all know which one we’d rather have on our side.

So how does one differentiate between these tissues?
Because the Soleus and Posterior Tibialis are the two usual suspects and responsible for the majority of problems when it comes to ankle dorsiflexion limitations, these two will usually require the majority of your focus both in evaluation palpation and treatment.
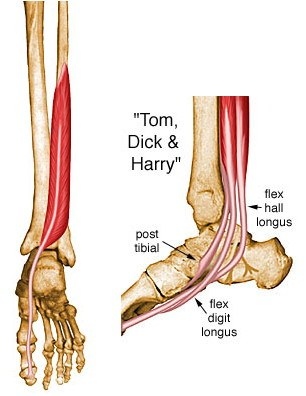
However, both the Flexor Hallucis Longus and the Flexor Digitorum Longus can limit dorsiflexion and should be excluded to be sure that they are not involved. To exclude these two structures from your list of possible dysfunctional contributors simply ask the patient to maximally dorsiflex their ankle while keeping their heel on the ground.
1. Gently pick up the great toe off the ground into extension. If there is slack and the patient does not indicate an increase in symptoms then the FHL is more than likely not involved.
2. Repeat tissue testing by selecting the toes and pulling them into extension. If there is slack and the patient does not indicate and increase in symptoms then the FDL is more than likely not involved.


To identify the underlying tissue whether it be the soleus or posterior tibialis requires some discernable palpation skills.
Did I make a permanent change?
Charlie Weingroff calls it the “Audit Process” while others such as good friend and colleague Pete Viteritti simply calls it, test-treat-retest. If the correct treatment choice was matched to the correct tissue choice and location then a marked improvement in range, function and/or pain levels should occur.
If minimal or no improvements were made than the following may have occurred:
1. You applied the correct treatment to the wrong tissue (tissue adhesion was within the posterior tibialis and you treated the soleus for example), or
2. You applied the incorrect treatment to the correct tissue (pressure was too light and thus was not sufficient to break up the underlying scar tissue), or
3. The limiting factor was not soft tissue but instead an osteokinematic “misalignment” or a position fault as described and made famous by Brian Mulligan (more Mulligan in a future post).
Summary: The most important step in any treatment approach starts with first identifying the correct pain generator or dysfunctional tissue involved. Without a correct place to start, all treatment options will fail to make a lasting change.
Topics: Art Horne, basketball conference, basketball training programs, athletic training conference, athletic training, boston hockey conference, Barefoot in Boston, Dorsiflexion, ankle problems
Posted by Boston Sports Medicine and Performance Group on Mon, Oct 3, 2011 @ 07:10 AM
by Art Horne
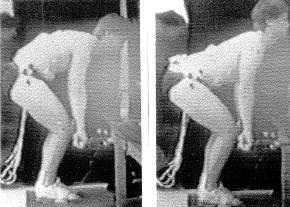
Last week we discussed the importance of bringing all professionals who care for and provide performance services to your student-athletes together to develop a consistent teaching methodology and progression to mastering the squat pattern. This week we look at the Hip Hinge.

Hip Hinge: all athletes should be able to separate their hips from a back strategy both in 2-legs and single leg stance -whether its knee, hip or other LE injury pain, we should be able to look at this movement pattern and address some overall concerns IN ADDITION to their traditional rehab program.
The hip hinge can be easily taught and standardized with our stick series.
Teaching Stick Series:
1. Stick maintains contact with three points (head, back and butt crack) throughout entire movement.
2. Reach butt backwards; knees should have slight bend.
3. Start with two feet on ground and progress to single leg stance.
4. This is not a squat pattern – be sure to hinge at the hips.
5. Maintain a packed neck (c-spine in-line with sternum throughout movement).
Start one foot away from wall (maybe just less) and reach back towards the wall with butt
1. Maintain three points of contact with stick on head, back and butt crack
2. This is not a squat pattern – first motion should be back towards the wall and not downwards.
3. Inch outwards from the wall with each successful repetition and repeat until you have found your end range.
4. ALTERNATIVE: face wall and touch with hands, move away from wall and repeat until you have reached max distance from wall while maintaining perfect form
Progression:
1. Two Leg Stick
2. SL Stick
3. 2-Leg – 2 hand Kettlebell Deadlift
4. SL 2-DB Deadlift
5. SL contralateral 1-DB Deadlift
When you finally get strength and sports medicine professionals together in the same room some amazing things begin to happen, especially when you start talking about hinging at the hips including:
1. Agreement to Pack the Neck: Packing the neck and maintaining a neutral cervical spine instead of admiring yourself in the mirror during a hip hinge stick series becomes a universal theme among both groups and taught and coached consistently – whether it’s pulling 300 pounds from the floor during a sumo squat or 4 weeks post ACL surgery during a simple stick series. Knowing where an athlete is going and where they’ve come from is half the battle in my opinion.
2. Glute activation takes on a whole new meaning to athletic trainers when they see firsthand the work and technical coaching that strength coaches employ with their athletes. Sets of 3x10 for glute bridges and then discharge to full participation is no longer acceptable.
3. Bad Hip Hinge means Bad Back: In the same breath, strength coaches are able to discuss challenges with low back pain patients with sports medicine professionals and appreciate how important they are in the rehabilitation and care of those persons as well as how incredibly dangerous a poorly performed lift can be.
Read article on Hip Hinge by clicking HERE.
Topics: basketball resources, basketball training programs, athletic training conference, athletic training, athletic training books, barefoot strength training, Hip Hinge, deadlift Art Horne
“The residents who live here, according to the parable, began noticing increasing numbers of drowning people caught in the river’s swift current and so went to work inventing ever more elaborate technologies to resuscitate them. So preoccupied were these heroic villagers with rescue and treatment that they never thought to look UPSTREAM to see who was pushing the victims in.”
Learn what is hurting your feet and your performance, and how to finally train your feet the way they were meant to be.
© 2020 Boston Sports Medicine and Performance Group, LLC