This is part 1 of the weekly “Friday Five” series where I ask 5 tough questions to world class elite coaches.
Irving "Boo" Schexnayder is regarded internationally as one of the leading authorities in training design, especially in the Jump events. He coached triple jumper Walter Davis, long jumper John Moffitt, and 19 NCAA Champions.
Boo will be speaking at the Boston Sports Medicine and Performance Group (BSMPG) on May 19-20, 2012.
You can also see his complete jumps DVD package for the Long, Triple and High Jump (plus a weight training bonus).
Q1 – SpeedEndurance.com: A lot of confusion and mystery lies with the true volumes of jump training that is sufficient for stimulating neuromuscular adaptions and teaching. While small doses are often looked at as the goal, teaching takes repetition. Could you expand on how important the sequence of the training year and the quality of foot strike? Can you explain why it seems that some programs thrive off of higher volumes while some just lead to injury?
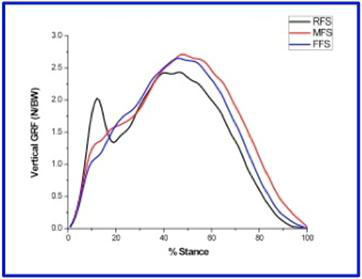
BOO: As far as foot strike, the ability to properly dissipate impact forces through full-footed landings is obviously a huge help to staying injury free while jump training. I think there are two other, more subtle keys to successful progression and remaining injury free in jump training. The first lies in variety, specifically advancing training cycles in a timely fashion. The other is taking a purposeful approach to the process.
Just as athletes do, we as coaches tend to settle into comfort zones. You get your athletes doing particular forms of jump training. Then, as mastery is approached, it’s time to move on to something else, but our natural tendency is to breathe easy and admire our work for a while. Periodic shifts in exercise choice, volume and intensity are critical, even though they might make life for the coach tougher. Successful higher volume programs do this and show a bit of a pioneer spirit.
Also, everything done must have a very specific purpose. That purpose might be establishing initial volumes, technical development, high end or low end elastic strength development, or whatever. It’s easy to fall into a “this is my fallback workout” philosophy if you are not targeting something specific. This is the primary rationale behind the small volume programs, and I think this is the key with high training age athletes who have already accumulated injuries and other physical issues over the course of a career.
In either case, whether it is failure to progress or mindless repetition, at this point jump training quits being a stimulus and becomes simply another piece of baggage that must be carried around that increases injury risk.
Q2 – SpeedEndurance.com: You mention that Olympic lifts are great harmonizing agents to a program. With your experience could you address what mechanisms and systems such as posture and coordination enable the lifts to transfer to sprinting and jumping?
BOO: The results I see in my program are the main reason I feel strongly about using Olympic lifts. I don’t want to give anyone the impression that I researched them first and then started to use them. My personal journey was more of a matter of seeing huge gains and then figuring out why.
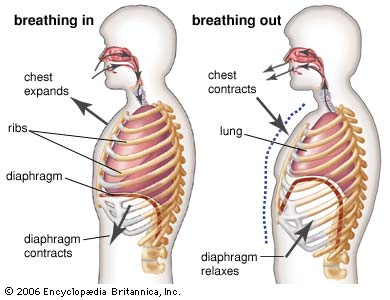
I think the orders of joint firing and the mixing of absolute strength, power, and eccentric activity show huge transfer into sport specific skills. Also, the need to stabilize the core while performing something functional like an Olympic lift does more for the body’s core than all the crunches in the world. In short, they are highly functional.
I am a fan of functional training. But I have never gone completely that way, always keeping a base in more old school approaches. Maybe it’s because I started my career in football, but it’s also because I have watched too many great athletes train that way to scrap it.
I think a key variable in strength training is the amount of muscle tissue activated in the course of a repetition. That variable, more than any other, affects blood chemistry and endocrine responses. Many exercises are functional but don’t elicit enough muscle fiber activation to accomplish this. Olympics are where gross movements meet functional training and old school meets new school.
Continue reading on speedendurance.com
See Coach Schexnayder at the 2012 BSMPG Summer Seminar as he talks, "Mulitjump Exercises: Applications for Teaching, Training, and Rehab"
Coach Schexnayder joins Chris Powers, Craig Liebenson, Bill Knowles, and Alan Grodin as Keynotes speaers. See these world class speakers along with the best Sports Medicine, Hockey and Basketball therapists and performance coaches throughout the weekend - May 19-20.
Register today before seats fill up!