by Art Horne

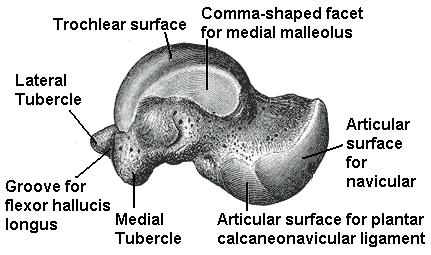
In a previous post we discussed how restrictions within the soft tissue surrounding the ankle joint may limit the ever so important motion of dorsiflexion. However, soft tissue dysfunction or tissue adhesions may not be the only limitation when it comes to you and your ankle joint moving freely. In fact, many times a gross reduction in motion may be caused by only a miniscule restriction in one of the surrounding foot and ankle bones, especially after injury.
This concept of “positional faults” was first made famous by Australian physiotherapist, Brian Mulligan in which he described an actual anterior translation of the fibula on the tibia after the typical inversion ankle sprain, rather than a disruption of the ATF ligament which so many athletic trainers and physical therapists focus their post-injury treatment protocol on.

“I believe that when the foot is forcibly plantar flexed and inverted beyond the natural range the lateral ligament usually suffers minor injury. The fibula gets wrenched forward on the tibia and positional faults occur.” (pg. 96 Manual Therapy by Brian Mulligan)
Mounting evidence is beginning to support this notion in some patients after the common ankle sprain as well as those with lateral ankle instability as indicated by the article summaries below. As with all your patient cases, a proper and methodical assessment is critical to determining if in fact a “positional fault” has occurred versus the previously discussed restriction within the soft tissue surrounding the ankle complex . In the event that a patient has difficulty after a “simple” ankle sprain, consideration should be given to Mulligan’s concepts with manual therapy techniques employed to correct these faults.
Fibular Position in Individuals with Self-Reported Chronic Ankle Instability
by Hubbard, Hertel and Sherbondy
It has been reported that 55% of individuals who sprain their ankle do not seek treatment and up to 70% suffer from repetitive sprains. Chronic Ankle Instability (CAI) may also lead to increased risk of osteoarthritis and articular degeneration. “Altered arthrokinematics lead to abnormal physiologic motions, distorted state of ligamentous structure and altered joint function” (pg.4), with the combination of these possibly leading to an increased risk of re-injury.
Purpose: The purpose of this study was to assess the position of the distal fibula in individuals with chronic ankle instability CAI.
Study Design: Thirty subjects with unilateral CAI and 30 subjects with no previous history of ankle injury participated in this study, completing a pair of subjective functional scales and fluoroscopic lateral images for both ankles with the distance from the anterior margin of the distal tibia to the anterior margin of the distal fibula measured.
Results: There were statistically significant differences in fibular position for the subjects with unilateral CAI compared to their non-injured limb as well as the control group, suggesting an anterior positional fault was present in those with unilateral CAI.
Conclusion: the fibula was positioned significantly more anterior in relation to the tibia in subjects with unilateral CAI but further research is needed to determine if repetitive bouts of ankle instability caused the anterior fibula position or if the position was a predisposing factor to injury.
______________________________________________________________________________
Clinical Pearl: Suspicion of fibula position fault should be high in lateral ankle sprains with longer than usual symptoms despite traditional treatment, especially in those ankles with swelling that remains despite treatment and is supported by Hubbard and Hertel 2008 in which they found, “a strong positive correlation between fibular position and swelling.” In addition, “those ankles with more swelling had the most anteriorly positioned fibulae. The fibulae in sub-acutely sprained ankles appear to be positioned more anteriorly compared to the contralateral ankles. This positional fault may be maintained acutely by swelling.” (pg. 63)
______________________________________________________________________________
Immediate Effects of Anterior-to-Posterior Talocrural Joint Mobilization after Prolonged Ankle Immobilization: A Preliminary Study
by Landrum, Brent, Kelln, Parente, Ingersoll and Hertel
Ankle dorsiflexion ROM typically decreases after prolonged immobilization and thus is a central focus for many clinicians during the rehabilitation process. Interventions such as static stretching and joint mobilizations are often employed as an effort to restore this very motion. “Passive mobilizations consist of gentle oscillating movements of the articular surfaces that create the movement of joints by a means other than the musculotendinous units that normally act on those particular segments. Joint mobilizations are purported to relieve pain and improve range of motion of injured joints. Such improvements can in turn lead to an increase in functional activities.” pg. 100.
Purpose: “The purpose of this study was to determine if a single bout of Grade anterior-to-posterior talocrural joint mobilizations immediately affected measures of dorsiflexion ROM, posterior ankle joint stiffness, and posterior talar translation in ankles of patients who have been immobilized at least 14 days.”
Study Design: The study used 10 subjects 5 male and 5 female each who had been previously immobilized following lower extremity injuries with at least a 5 degree deficit in ankle dorsiflexion. Immobilization ranged from 2 weeks to 9 weeks. All subjects underwent three series of measurements of ankle dorsiflexion ROM, posterior talar mobility, and posterior joint stiffness. ROM was measured using a bubble inclinometer and talar mobility and joint stiffness were measured using an ankle arthrometer. The subjects were split into two groups one receiving the intervention and one control group. All subjects received both the joint mobilization and control (no intervention) in their crossover design.
Results: Ankle dorsiflexion ROM increased significantly at each assessment period. A possible reason for this increase in dorsiflexion ROM could be due to correction of an anterior positional fault of the talus after joint mobilizations. It is possible that these faults were corrected via either the joint mobilization and/or the arthrometer testing.
Conclusion: “After a single application of Grade III anterior-to-posterior talocrural joint mobilization, dorsiflexion ROM and posterior ankle joint stiffness were significantly increased. There was also a trend toward less posterior talar translation immediately after immobilization.” This result may be related to correction of a positional fault at the talocrural joint.
______________________________________________________________________________
Interesting Note: “Mulligan’s positional fault theory may help explain our findings. Residual loss of the posterior glide may be representative of an anterior positional fault of the talus on the tibia and may result in an abnormal axis of talocrural rotation. Through an acute mechanism of injury, such as ankle sprain, the talus may anteriorly subluxate and become stuck, thus resulting in restricted posterior glide and compromised ankle function. It is possible that the patients in our study who were immobilized for a prolonged period of time also developed positional faults of the talus and that these positional faults were corrected via either the joint mobilizations and/or the arthrometer testing.” pg. 104
______________________________________________________________________________
Predicting Short-Term Response to Thrust and Nonthrust Manipulation and Exercise in Patients Post Inversion Ankle Sprain
By Witman et al.
“It has been estimated that the reinjury rate following a lateral ankle sprain may be as high as 80% suggesting the need to identify the most effective management strategies for this condition.”
Purpose: The purpose of this study was to develop a clinical prediction rule (CPR) to identify patients who had sustained an inversion ankle sprain who would likely benefit from manual therapy and exercise.
Study Design: Consecutive patients with a status of post inversion ankle sprain underwent a standardized examination to determine baseline data followed by a treatment program consisting of ankle/foot thrust and non-thrust manipulation, general mobility exercises (including ROM and stretching), advice to maintain usual activity within the limits of pain, and instruction in the use of ice and elevation. Thrust manipulations included a rearfoot distraction technique and a proximal tibiofibular joint posterior-to-anterior thrust manipulation. Nonthrust manipulation techniques used included anterior-to-posterior talocrural technique, lateral glide/eversion rearfoot technique and a distal tibiofibular technique. Of the 85 patients enrolled in the study, 64 or 75%, experienced a successful outcome as reported on the Global Rating of Change scale. Of those who experienced success, 35 or 55%, experienced a successful outcome at the time of the second visit and the remaining 29 experienced success at the 3rd visit.
Conclusion: The study developed a CPR to identify patients with a status of post inversion ankle sprain who would most likely benefit rapidly and dramatically from manual therapy and general exercise. If 3 of the 4 variables (symptoms worse when standing, symptoms worse in the evening, navicular drop >5 mm, or distal tibiofibular joint hypomobility), were present, the accuracy of the rules was maximized and the post-test probability of success increased to 95%.
______________________________________________________________________________
Interesting Note: Athletes/patients who have suffered ankle sprains in high school and did not seek medical help but instead left their ankle trauma to resolve on its own, often present years later with limited ankle range of motion with associated knee or other foot pain for which they usually present. It is this author’s experience that athletes with previous ankle sprains, but otherwise “healthy” benefit greatly from the following mobilization techniques (described in this article) as part of their comprehensive treatment in an effort to regain normal ankle dorsiflexion regardless of their initial presentation.
Appendix A – page 199
• Lateral Glides and Eversion Mobilization/Manipulation to the Subtalar Joint
• Talocrural joint Anterior-to-Posterior mobilization/manipulation with patient supine and ankle off end of treatment table
• Talocrural joint Anterior-to-Posterior mobilization/manipulation (mobilization with movement utilizing belt for assistance)
** This is true for both acute ankle inversion sprains as well as for athletes with residual restrictions from prior injury. In a study by Green et al., in 2001 the addition of talocrural mobilizations to traditional RICE protocols necessitated fewer treatments to achieve pain-free dorsiflexion.
______________________________________________________________________________
Initial Changes in Posterior Talar Glide and Dorsiflexion of the Ankle After Mobilization With Movement in Individuals With Recurrent Ankle Sprain
By Vicenzino et al.
“Physiotherapists frequently use mobilization with movement (MWM) techniques as a physical treatment to improve range of motion, alleviate pain, and promote earlier return to function following lateral ankle sprain.”
Purpose: Test current contention that mobilization with movement (MWM) to the talocrural joint in both weight bearing and non–weight bearing positions improve posterior talar glide as a means to increasing ankle dorsiflexion
Study Design: 8 females and 8 males ages 18-27 recruited from Queensland’s student population
• Inclusion Criteria: “history of recurrent ankle sprain with at least 2 ankle sprains, more than 20 mm asymmetry on the weight-bearing lunge test for ankle dorsiflexion, no history of lateral ankle sprain on the contralateral side, and not receiving any other physiotherapy treatment during the study”
• Exclusion Criteria: “acute ankle sprain within past 6 months, previous injury or surgery in the back, hip or knee, or major fracture to the ankle or distal leg”
Results: “weight-bearing and non-weight-bearing MWM treatment techniques both produced significant changes in posterior talar glide that were not evident in the control condition”
- Non-weight-bearing: “reduced posterior talar glide deficit by 50%”
- Weight-bearing: reduced posterior talar glide deficit by 55%
- Control: “reduced posterior talar glide deficit by 17%”
- Weight-bearing and nonweight-bearing MWM treatment improved weight-bearing dorsiflexion by 26%, compared to 9% by the control group.
Conclusion: “application of MWM treatment techniques improved posterior talar glide and talocrural dorsiflexion immediately after application in subjects with chronic recurrent lateral ankle sprain.”
____________________________________________________________________
Note:
“Approximately 44% of all sprained ankles go on to have further problems and although the factors that predispose to injury or reinjury are not conclusively evidence based, they are reported to involve proprioceptive deficits of the ankle, lack of ankle dorsiflexion, and reduced posterior glide of the talus in the ankle mortice.” (pg. 465)
“Denegar et al found a reduction in posterior glide of the talus in the ankle mortise in asymptomatic fully functional subjects in the 6 months following ankle sprain. It was postulated that because the talus lacks muscular attachments, it might subluxate anteriorly following disruption to the ligaments that attach to it. The talus then remains malpositioned anteriorly until it is passively returned to its ‘normal’ position. To an extent, the findings of reduced posterior talar glide and dorsiflexion range of motion appear congruent, as posterior talar glide is an accessory motion component of ankle dorsiflexion.” (pg. 465)
______________________________________________________________________________
Conclusion: Whether you are treating an acute ankle sprain, or addressing knee pain secondary to restricted ankle dorsiflexion a detailed evaluation which involves ALL contributing factors, both bony and soft-tissue, associated with a decrease in ankle dorsiflexion as outlined here and our previous post is the only way to ensure your patient will receive the best possible outcome and the fastest track back to normal function and high performance activities. Positional faults are impossible to find if you never look for them - assessment of all ankle sprains or ankles with limited motion should include a detailed examination of all bones related to the foot and ankle including the distal tib-fib joint and talus for appropriate accessory motions. In a future post I’ll discuss why the all so common, “ice and e-stim approach” to ankle sprain management only works for so long and why hip strength may actually be more important.
References
Collins N, Teys P, Vicenzino B. The initial effects of a Mulligan’s mobilization with movement technique on dorsiflexion and pain in subacute ankle sprains. Manual Therapy 2004; 9:77-82
Denegar, C., Hertel, J., Fonesca, J. The Effect of Lateral Ankle Sprain on Dorsiflexion Range of Motion, Posterior Talar Glide, and Joint Laxity. J Orthop Sports Phys Ther. 2002; 32(4):166-173.
Hubbard T, Hertel J, Sherbondy P. Fibular position in individuals with self-reported chronic ankle instability. J Orthop Sports Phys Ther. 2006;36(1):3-9.
Hubbard TJ, Hertel J. Anterior positional fault of the fibula after sub-acute lateral ankle sprains. Manual Therapy. 2008;13:63-67.
Landrum E, Kelln B, Parente W, Ingersoll C, Hertel J. Immediate effects of anterior-to-posterior talocrural joint mobilization after prolonged ankle immobilization: a preliminary study. J Manual Manip Ther. 2008;16(2):100-105.
Whitman J, Cleland J, McPoil T, et al. Predicting short-term response to thrust and nonthrust manipulation and exercise in patients post inversion ankle sprain. J Orthop Sports Phys Ther. 2009;39(3):188-200.
Vincenzino, B., Branjerdporn, M., Teys, P., Jordan, K. Initial Changes in Posterior Talar Glide and Dorsiflexion of the Ankle after Mobilization With Movement in Individuals with Recurrent Ankle Sprain. J Orthop Sports Phys Ther. 2006;36(6):464-471.
Green., T., Refshauge, K., Crosbie, J., Adams, R. A randomized controlled trial of a passive accessory joint mobilization on actue ankle inversion sprains. Phys Ther. 2001;81(4):984-994.
Mulligan BR. Manual therapy: “NAGS,” “SNAGS,” “MWMS,” etc. 3rd ed. Wellington, New Zealand: Plane View Services LTD; 1995.